Notes: The following information is intended for health care professionals. Always read the label and follow the instructions for use. For information on the efficacy and the side effects, refer to the instructions for use. Products are only for sale to health professionals.
What is Hip Dislocation?
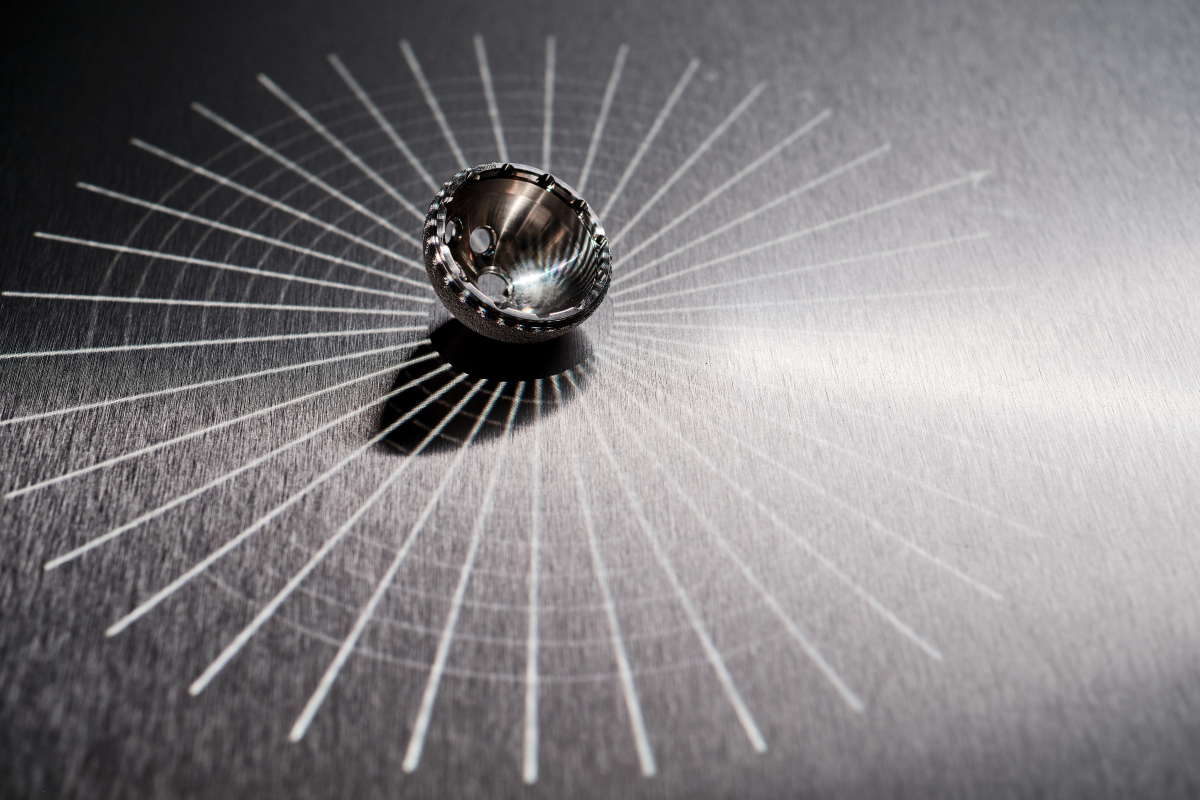
A hip dislocation after total hip replacement occurs when the femoral component moves out of the acetabular component. That is, the femoral head is no longer within the acetabular cup. A dislocation can be seen in the below radiograph from Dargel, et al.1.

How Is Hip Dislocation Treated?
Dislocations can be resolved in multiple ways:
Closed reduction: The femoral head is manipulated back into the acetabular cup without surgery,
Revision surgery: The surgeon replaces some or all components with further surgery,
Spontaneous recovery: The dislocation resolves without treatment.
Why do Hip Dislocation Rates Vary?
In individual studies, the measured dislocation rates vary widely and are affected by many factors. Rates have been reported from 0.5% through to 11%2-5. This wide range may be attributed to varying measurement methods (such as the timing of the assessment relative to the surgery), surgical materials and techniques (such as surgical approach, femoral fixation, and femoral head size), and patient characteristics (such as age, gender, body mass index [BMI], and comorbidity severity)3-7. The root of some of this variation may be country to country differences: a study analysing registry data found that the practices (such as surgical approach, head sizes, and fixation method) and patient characteristics (such as comorbidities) varied significantly between Sweden, Australia, and the United States8.
As an example of the complexity of measuring dislocation rates, consider the effect of soft tissue repair on dislocation for the posterior approach. In Australia and the Netherlands, the rate of revision due to dislocation was significantly higher for the posterior approach compared with the anterior and lateral approaches6, 7. Similarly, a systematic review by Berstock, et al.9 found a significantly higher rate of revision for the posterior compared with the lateral surgical approach. However, a systematic review by Kwon, et al.10 found that soft tissue repair reduced the risk of dislocation for the posterior approach by a factor of 8.21. Therefore, the differences between surgical approaches would be strongly influenced by the extent of soft tissue repair.
Are Dislocations Underreported?
In addition to being multiply influenced, dislocations appear to be underreported. Despite improvements in classification through using the International Classification of Diseases (ICD-10), registry records may not be complete11, 12. Underreporting was highlighted in a nationwide study comparing the Danish Hip Arthroplasty Register with a detailed review of patient files for 31,105 primary THAs11. Based on the comparison, there were 50% more dislocations in the patient files than in the registry data, illustrated below.
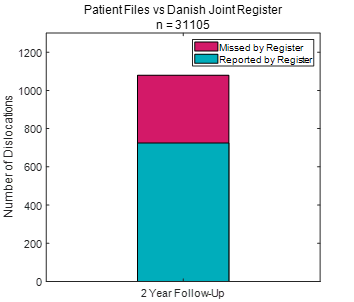
The authors argued that closed reductions may not be reported in registers, particularly if they do not require hospital admission or are treated somewhere other than the original hospital11. Typically, registries measure revision for dislocation, not dislocation. Consequently, if a dislocated hip were reduced in the emergency department or operating theatre, this intervention would not be recorded in a registry. Dislocations may also not be captured in registry data if the patient recovers spontaneously, goes to a different surgeon, or is not suitable for revision surgery. Therefore, dislocation may be a substantially larger problem than indicated by registry data.
Summary
Hip dislocations and their measurement are influenced by multiple factors and may be underreported in registry data.
References
- Dargel J, Oppermann J, Brüggemann G-P, et al. Dislocation following total hip replacement. Dtsch Arztebl Int 2014;111(51-52):884-90. doi: 10.3238/arztebl.2014.0884
- Lu Y, Xiao H, Xue F. Causes of and treatment options for dislocation following total hip arthroplasty. Exp Ther Med 2019;18(3):1715-22. doi: 10.3892/etm.2019.7733 [published Online First: 2019/07/03]
- Gromov K, Troelsen A, Otte KS, et al. Removal of restrictions following primary THA with posterolateral approach does not increase the risk of early dislocation. Acta Orthop 2015;86(4):463-8. doi: 10.3109/17453674.2015.1028009 [published Online First: 2015/03/11]
- Malkani AL, Ong KL, Lau E, et al. Early- and late-term dislocation risk after primary hip arthroplasty in the Medicare population. J Arthroplasty 2010;25(6 Suppl):21-5. doi: 10.1016/j.arth.2010.04.014 [published Online First: 2010/06/15]
- Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Hip, Knee & Shoulder Arthroplasty: 2019 Annual Report. 2019
- Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Hip, Knee & Shoulder Arthroplasty: 2020 Annual Report, 2020.
- Zijlstra WP, De Hartog B, Van Steenbergen LN, et al. Effect of femoral head size and surgical approach on risk of revision for dislocation after total hip arthroplasty: An analysis of 166,231 procedures in the Dutch Arthroplasty Register (LROI). Acta orthopaedica 2017;88(4):395-401. doi: 10.1080/17453674.2017.1317515
- Paxton EW, Cafri G, Nemes S, et al. An international comparison of THA patients, implants, techniques, and survivorship in Sweden, Australia, and the United States. Acta Orthopaedica 2019;90(2):148-52. doi: 10.1080/17453674.2019.1574395
- Berstock JR, Blom AW, Beswick AD. A systematic review and meta-analysis of complications following the posterior and lateral surgical approaches to total hip arthroplasty. Ann R Coll Surg Engl 2015;97(1):11-16. doi: 10.1308/003588414X13946184904008
- Kwon MS, Kuskowski M, Mulhall KJ, et al. Does surgical approach affect total hip arthroplasty dislocation rates? Clin Orthop Relat Res 2006;447:34-8. doi: 10.1097/01.blo.0000218746.84494.df [published Online First: 2006/06/03]
- Hermansen LL, Viberg B, Hansen L, et al. “True” Cumulative Incidence of and Risk Factors for Hip Dislocation within 2 Years After Primary Total Hip Arthroplasty Due to Osteoarthritis: A Nationwide Population-Based Study from the Danish Hip Arthroplasty Register. J Bone Joint Surg Am 2021;103(4):295-302. doi: 10.2106/JBJS.19.01352
- American Academy of Orthopaedic Surgeons. The Seventh Annual Report of the AJRR on Hip and Knee Arthroplasty, 2020.