Notes: The following information is intended for health care professionals. Always read the label and follow the instructions for use. For information on the efficacy and the side effects, refer to the instructions for use. Products are only for sale to health professionals.
In Brief
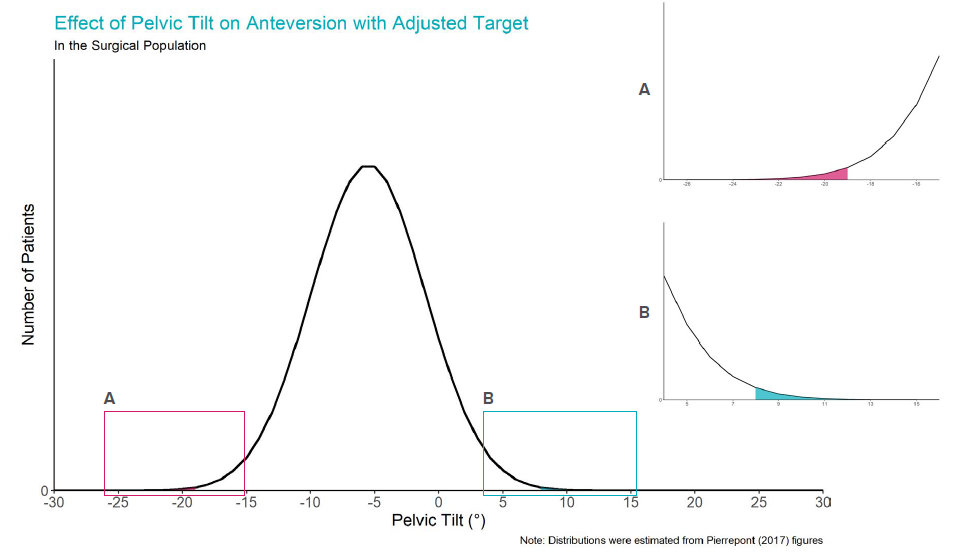
A target cup position of 39° inclination and 16° anteversion could accommodate standing-to-supine pelvic tilt for the patient population in a recent study1. Using this adjusted target and a functional reference plane, 99.7% of patients are projected to be within ± 10° of the target for anteversion. Keep reading to find out why.
What is Pelvic Tilt?
The anterior pelvic plane is defined using the anterosuperior iliac spines (ASISs) and the pubic symphysis.
 Pelvic tilt may be measured as the tilt of the anterior pelvic plane relative to the coronal plane2, shown here for a standing patient.
Pelvic tilt may be measured as the tilt of the anterior pelvic plane relative to the coronal plane2, shown here for a standing patient.

Does Pelvic Tilt Vary?
The Patient Population
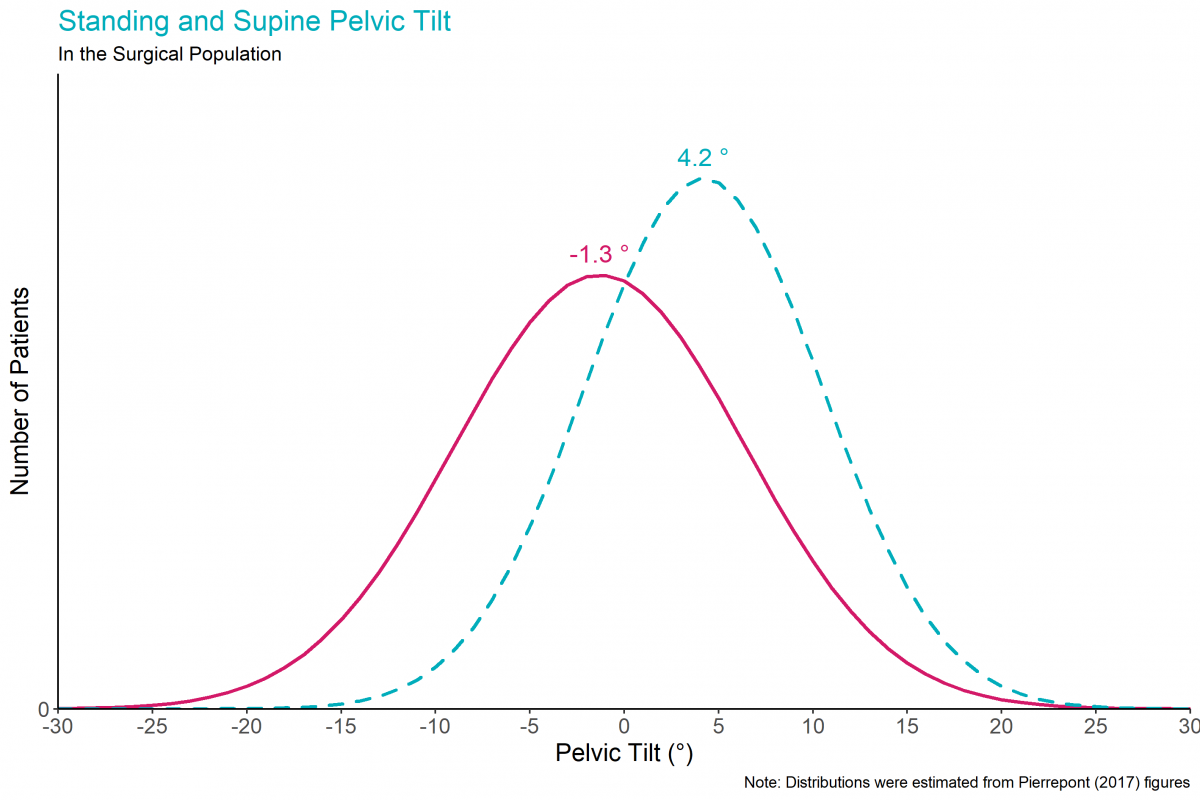
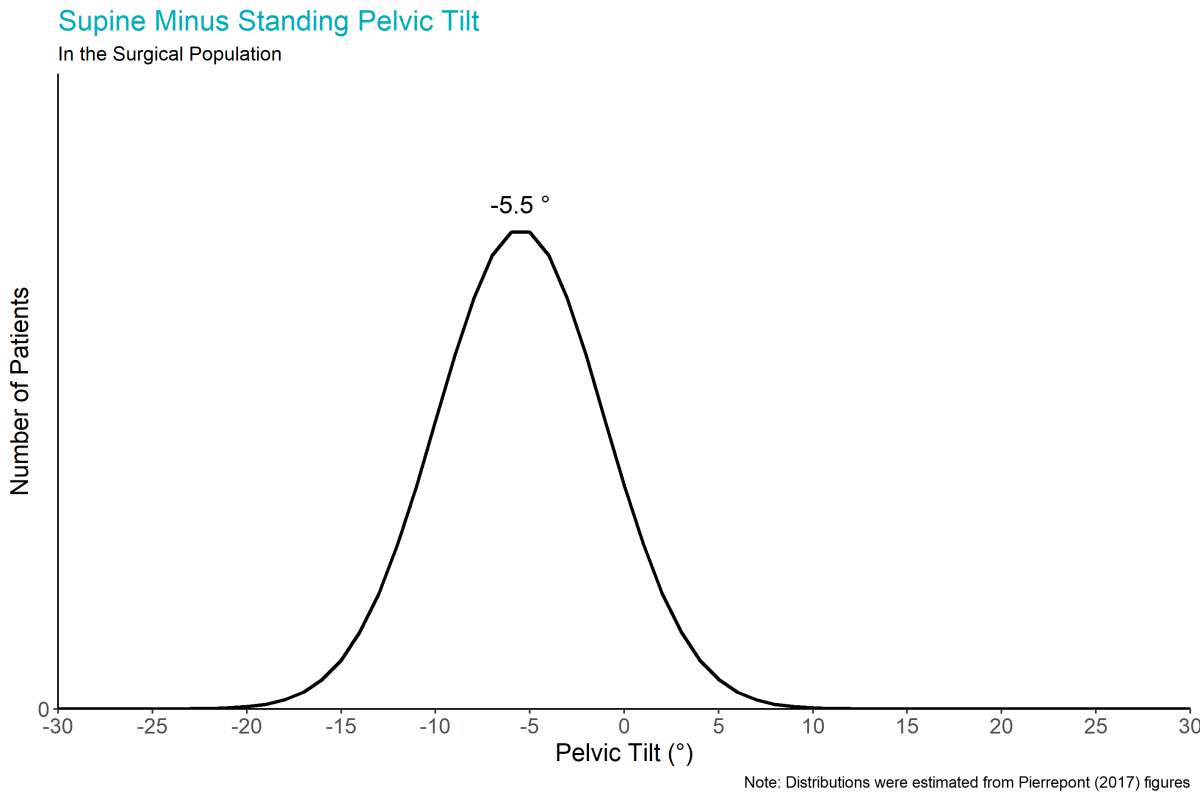
Patients vary in their standing pelvic tilt, supine pelvic tilt, and the difference between standing and supine pelvic tilt. We illustrate this variation by using normal distributions to approximate the data from a study of 1517 patients1, with positive angles representing anterior pelvic tilt.
These patients were from consecutive Australian surgeries in 2014 and 2015, with an average patient age of 63 years and with 53% male, 47% female.
The Average Patient
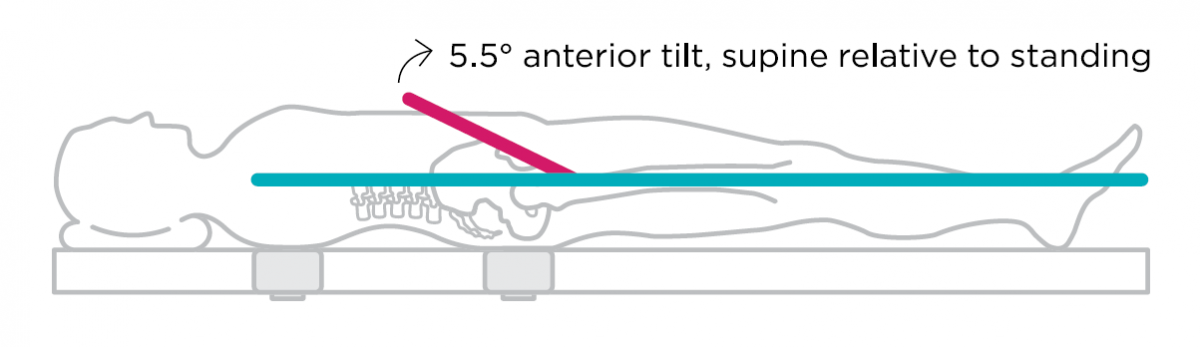
The pelvis typically tilts between the supine and standing positions1, 3. The average patient has 4.2° of anterior pelvic tilt when supine, 1.3° of posterior pelvic tilt when standing, and therefore, 5.5° of posterior pelvic tilt when they go from supine to standing1, 3.
Why is Pelvic Tilt a Potential Concern?
With surgery in the supine position and the target acetabular cup orientation in the standing position, a potential concern is the effect of this supine-to-standing pelvic tilt on post-operative cup position. This effect can be quantified using the definitions provided by Murray4. A relative posterior change in pelvic tilt of 13° from supine to standing would increase the anteversion of the acetabular cup by 10°. Based on the above patient population, 6% of patients would have unacceptably high anteversion.
Adjusting the Intraoperative Target
It is possible to adjust the intraoperative (supine) target for acetabular cup position so that the average patient has a 40°/20° post-operative (standing) cup position.
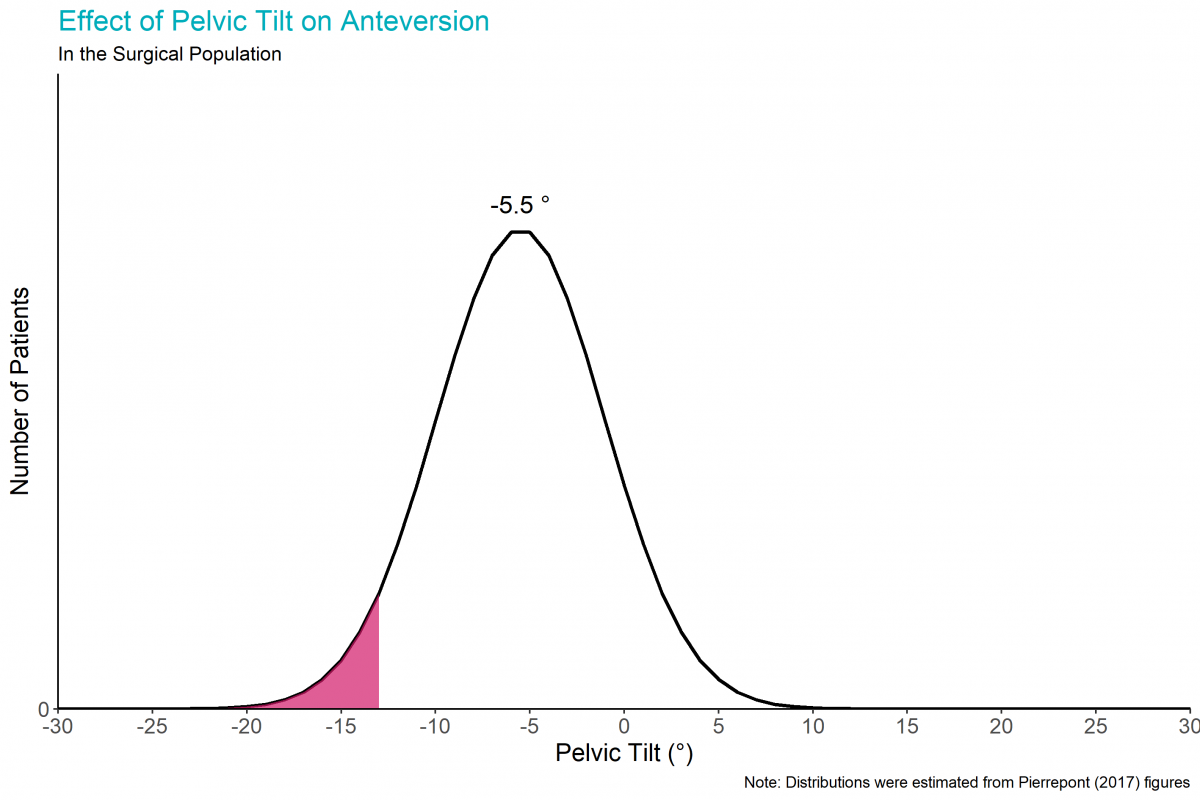
Using Murray’s definitions4, with no adjustment (i.e. an intraoperative target of 40°/20°), the average patient (with a 5.5° posterior pelvic tilt from supine to standing) has a projected post-operative acetabular cup position of 41°/24°. For this average patient, adjusting the intraoperative acetabular cup target to 39°/16° leads to a predicted post-operative acetabular cup position of 40°/20. Thus, a 39°/16° target achieves the desired outcome for the average patient.
What about the patient population? Using the 39°/16° intraoperative target centres the patient distributions around -5.5°. The pelvic tilts that result in ±10° post-operative anteversion are then -18.7° and 7.7°. The areas of the patient population outside of these limits are so small that they are barely discernible. In fact, using the adjusted target, an estimated 0.3% of the population would have an absolute change in anteversion greater than 10°.
Summary
For the patient data that were analysed here, a target cup position of 39° inclination and 16° anteversion with a functional reference plane can accommodate standing-to-supine pelvic tilt. Using this adjusted target, 99.7% of patients are projected to be within the target of ± 10° for anteversion. Appropriate caution should be used in applying the learnings from this patient group to other patient demographics.
References
- Pierrepont J, Hawdon G, Miles BP, et al. Variation in functional pelvic tilt in patients undergoing total hip arthroplasty. Bone Joint J 2017;99-b(2):184-91. doi: 10.1302/0301-620x.99b2.Bjj-2016-0098.R1 [published Online First: 2017/02/06]
- Harrison CL, Thomson AI, Cutts S, et al. Research Synthesis of Recommended Acetabular Cup Orientations for Total Hip Arthroplasty. The Journal of Arthroplasty 2014;29(2):377-82. doi: 10.1016/j.arth.2013.06.026
- Buckland AJ, Fernandez L, Shimmin AJ, et al. Effects of sagittal spinal alignment on postural pelvic mobility in Total Hip Arthroplasty candidates. The Journal of Arthroplasty 2019;34(11):2663-68. doi: 10.1016/j.arth.2019.06.036
- Murray DW. The definition and measurement of acetabular orientation. Journal of Bone & Joint Surgery 1993;75(2):228-32. doi: 10.1302/0301-620x.75b2.8444942 [published Online First: 1993/03/01]